ABDOMINOPLASTY/
MOMMY MAKEOVER

I am not going to bore you with countless before and afters here. This section is geared to young surgeons curious to improve their skills and outcomes. We will explore a better belly button, advantages of the horizontal mattress suspension stitch, complication rates of out-patient surgery vs inpatient, and incision placement. Graphic surgical video is presented for teaching purposes.
BELLY BUTTON byVillar
Embarking in private practice in 1982, I was preocuppied with solving the main cosmetic flaw in abdominoplasty, the UGLY belly button scar.
When the unsightly supra-pubic scar was cleverly hidden beneath the bikini tan line, only the belly button scar was exposed for all the world to see.
The standard of practice was to cut around the original belly button and preserve the long stalk down to the abdominal wall. After the abdominal wall was plicated and the supra-umbilical skin was pulled down, a new button hole was made in the skin and the original stalk was pulled up through it and sutured in place. This left the scar on the surface, and caused me sleepless nights. Now that I was the boss in private practice, I experimented with various options. The final solution was so logical, it evaded discovery before much trial and error. I will skip to the evolution. After the diastasis (weakness in midline due to lateral separation of the rectus muscles and thinning of midline fascia) was repaired with a suspension bridge horizontal mattress suture, The remaining umbilical stalk was evaluated. It was then cut very close to its base. Instead of bringing the long stalk up to the surface, the surface was brought down to the short base. This was best accomplished with a short vertical incision, removing a small cone of fat beneath the incision, and placing four oriented silk sutures in the stump from underneath up through the hole at four quadrants before laying the flap down. once the flap was secured, the sutures were tightened bringing the skin down to the base , minimizing an ugly scar. Packing was inserted to maintain the shape.
That was a fun and rewarding journey to find a better way.
THE DIBENEDETTO HORIZONTAL MATTRESS SUTURE byVillar
Anthony DiBenedetto was the most respected general surgeon on Long Island. As my Chief of Surgery, he taught me how to close every abdominal incision, including dehisced wounds, with a horizontal mattress suture instead of the standard individual sutures. His concept was that interrupted sutures are subject to the uneven stress of movement. When you sit up, stress transitions up and down your abdominal wall. Interrupted sutures can tear out or break when uneven stress reaches them especially in the presence of weak or devascularized tissue. We had witnessed massive abdominal wall tissue loss and necrosis in patients with infected mesh.
His philosophy was NEVER USE MESH. His solution was the horizontal mattress suture which acts as a suspension bridge. The heavy nylon actually slides back and forth, evenly adjusting to the varying tension. This repair never failed during my two years with him even in the monster cases.
I have never used Mesh and adopted it to my abdominoplasties and abdominal wall reconstructions without failure.
The technique in abdominoplasty involves starting supra-pubic with an over and over technique up to the umbilical stump, around it to avoid chocking blood supply, then up to the xyphoid. The origin is clamped, not tied. This provides the initial tightening. The suture is brought back down in a horizontal mattress fashion through the outer rectus fascia, fine tuning the tightening to drum tight while still under muscle paralysis. The suture leaves room around umbilical stump, then down to the supra-pubic origin. The origin suture and the returning suture are pulled tight and snugged up before tying to each other. This suture is very slippery , so I place fifteen knots, and bury them under the repair with a long thin right angle clamp leaving long ends to prevent unravelling. This repair is an engineering marvel and likely did not mainstream with the advent of endoscopic surgery in general surgery.
HOSPITAL vs OUT-PATIENT
In my opinion, there is no question the in-hospital abdominoplasty with a three day in hospital stay is safer and more comfortable than out-patient care. The problem is that only my very wealthy patients can afford the exorbitant cost of nearly twenty thousand dollars.
Our complication rate has been under 1% and we have not lost any skin since 1983. Out-patient surgery complications are often mentioned about 15%, but we really don’t know because nobody is reporting these complications honestly in the outpatient setting. I have not had a slough since 1983 , but I have treated dozens because when patients have a serious complication they loose trust in their surgeon and come to me and others for a second opinion. Reviewing the medical records, none of these complications were reported to anyone.
LEAVE FLAPS UNTILL THE END
Delicate tissue dissection and tissue handling is critical to tissue healing, low infection rates, and standard swelling resolution. The more tissue damage, the more complications. The excess tissue that will be cut off should be left to the very end. It can be grabbed, clamped and retracted without compromising the suture line.
SCARPA’S FASCIA IS IMPORTANT
My experience is that there is a fatty layer above Scrapa’s facia and a fat layer beneath it, contrary to many diagrams on the Internet. The importance of this layer is that it must be identified and repaired to restore its integrity to minimize depressed scars typically seen in hysterectomy scars and infra-mammary scars. It is easily identified as a strong white layer capable of holding a suture without tearing. It can be tinted with a marker before cutting through, to better identify it for repair on the way out.
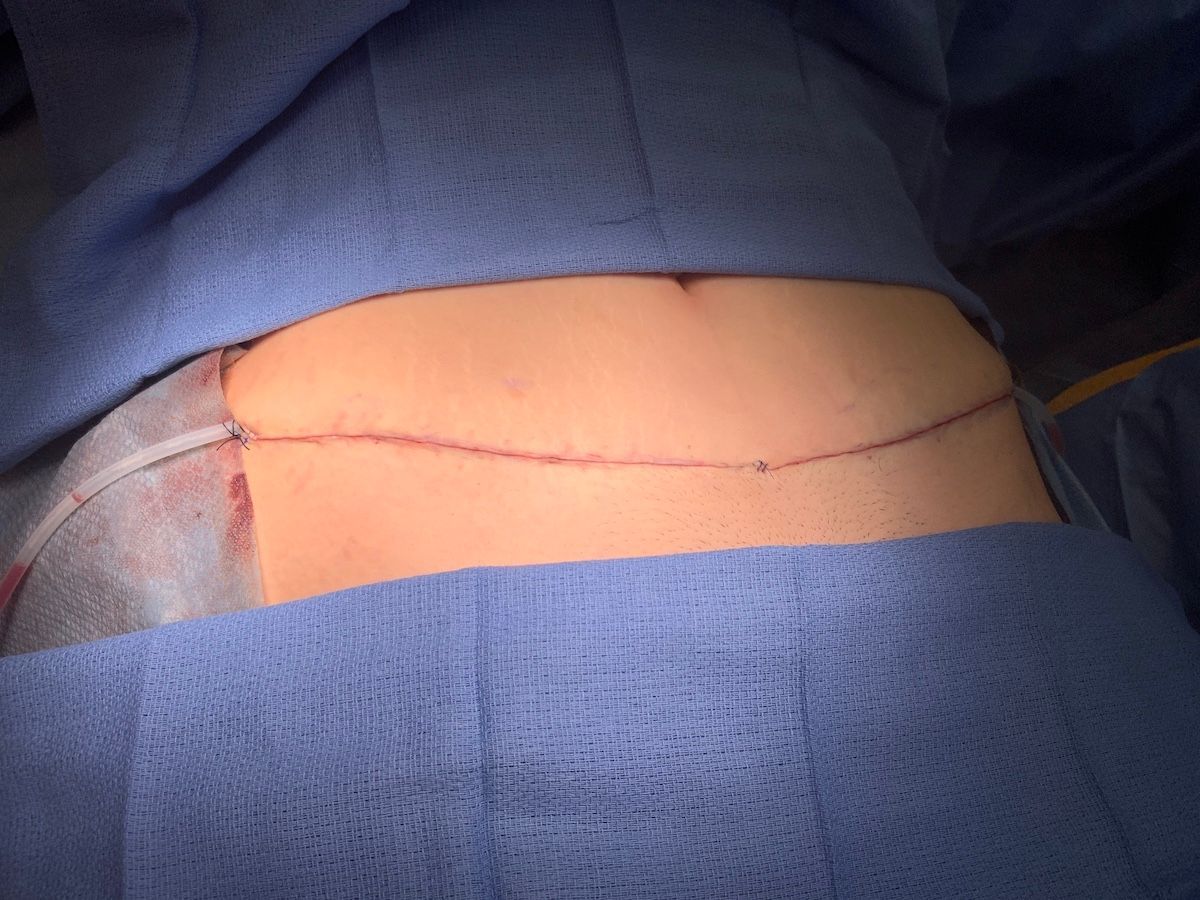
After Scrapa’s fascia is repaired with a running 3-0 Vicryl, a 10mm flat drain is slid under it laterally. Then the skin is approximated with 4-0 Vicryl dermal sutures with the knots buried. If the suture is pulled parallel to the skin when cinching down the knot, the skin edges should come together perfectly , if properly placed. Some practice is required. Now a running sub-cuticular suture is placed to provide a closure without “railroad track” scars. We used to reinforce with a few cross sutures and remove them at five days, but now we just glue over the subcuticular suture.
The key to success in repairing supra-pubic incisions is suturing Scarpa’s fascia and restoring it’s integrity. C-section scars such as this one that are fused to the abdominal wall cause the tissue to roll over the incision line because the natural ability of the skin to slide back and forth is thwarted.
We usually find the skin scar goes straight down to the abdominal fascia. We cut this out back to normal tissue, then identify Scarpa’s fascia which separates a superficial layer of fat and a deep layer of fat. Repairing this separates the fat layers and minimizes the chance of a solid scar mass through all layers recurring. In this case we removed a large amount of redundant tissue which is not common in most of the smaller depressed C-section scars. In cosmetic cases, we use a running sub-cuticular suture to avoid cross hatch railroad track scars.
REALITY CHECK
No matter how meticulous the technical mastery of the surgery, which is totally under control of the surgeon, there comes the healing phase which has a mind of its own. Every patient heals differently depending on the mysteries of their genetic code.
The best we can do is set up the conditions for optimal healing, (delicate tissue handling, tissue plane dissection, atraumatic suture techniques, drains, dressings, etc.) and the rest is up to nature.
Identifying potential complications early (hematomas, cellulitis, hypertrophic healing, allergic reactions, etc.) and dealing with them before they progress to disasters requires checking the patient the day after surgery now that in-hospital observation and recovery is unaffordable.
We have seen some rare but crazy anomalies and fortunately had the training and experience and luck to deal with them without worsening the condition.
We are based in:
421 SE Osceola St.
suite A Stuart,
FL, US 34994
Call us:
Email us:
All Rights Reserved | Villar Plastic Surgery | Privacy Policy




